AUTOMATED PRIOR AUTHORIZATION
Streamlining Specialty Medication Management Under Medical Benefits
Reduce Administrative Hurdles to Fast-Track Time to Therapy

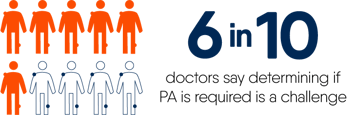
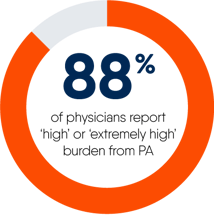
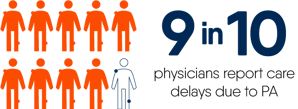
As specialty medications grow at twice the rate of traditional medications, insurance coverage complexity presents an increasingly significant obstacle faced by providers, staff teams, and patients when starting prescribed therapies. Barriers like complex prior authorization (PA) workflows become roadblocks to patient access and adherence.
1
Now, whether drugs fall under pharmacy or medical benefits, you can create a more efficient automated prior authorization workflow for your users and smoother care pathways for their patients.
Unlike standardized e-Prescribing processes under pharmacy benefits, medical benefit PAs have no universal standard. Instead, 68%2 of PAs under medical benefits rely on inefficient manual or only partially electronic processes.
Automation and AI advancements address complexity, supporting seamless data exchanges and efficient workflows that pave the way for patients to get and stay on prescribed therapies.
1 American Medical Association. 2023 AMA Prior Authorization Physician Survey. United States of America: AMA; 2024. https://www.ama-assn.org/system/files/prior-authorization-survey.pdf. Accessed August 7, 2024.
2 The Council for Affordable Quality Healthcare®. 2023 CAQH Index Report: A New Normal: How Trends From the Pandemic Are Impacting the Future of Healthcare Administration. CAQH; 2024.
ON-DEMAND WEBINAR
Unlock expert insights on tackling specialty medication challenges—including regulatory requirements—and learn how automation can streamline access and improve patient outcomes.
With flexible implementation options, including APIs, SMART® on FHIR®, and more, DrFirst streamlines workflows and delivers an enhanced user experience to:
- Improve communication and care coordination between providers, payers, and patients with transparent and timely updates, providing clear timelines and reducing uncertainty
- Streamline complex specialty medication PAs, reducing manual effort by 70% or more
- Eliminate up to 90% of PA claims rework due to preventable denials by prechecking for errors or omissions
- Shrink authorization cycle time up to 90%, speeding up patients’ time to therapy
Accelerate the end-to-end process—from benefit verification and patient financial responsibility calculation through prior authorization submission and status monitoring in minutes.
Join the shift towards smarter, proactive medication management that keeps the focus on patients, not paperwork.


